
Most pet owners believe bad breath is normal, but it’s the primary warning sign that your pet’s mouth has become a gateway for systemic disease that can shorten their life.
- Bacteria from infected gums directly travel through the bloodstream, seeding infections in the heart, kidneys, and liver.
- Many “dental chews” provide a false sense of security, failing to clean below the gumline where the real danger lies.
Recommendation: Shift from passively managing bad breath to proactively disrupting oral biofilm through daily brushing and annual professional cleanings under anesthesia—it’s the single most effective action you can take to protect their overall health and longevity.
As a veterinary dentist, I see a common, heartbreaking pattern every day. A loving owner brings in their dog, often for a routine check-up, and mentions the “doggy breath” as if it’s an unchangeable fact of life. They’ve accepted it. They buy breath-freshening treats and hope for the best. What they don’t realize is that this odour isn’t just unpleasant; it’s a distress signal. It’s the scent of active periodontal disease, a chronic infection that is quietly seeding bacteria throughout their pet’s body and shaving years off their life.
The conventional wisdom is to offer a dental chew or use a water additive. While some products have a place, this approach often misses the root of the problem. It’s like trying to fix a crumbling foundation with a coat of paint. The real issue lies beneath the surface, in the sticky, invisible layer of biofilm where bacteria multiply. This is where the battle for your pet’s health is won or lost. The bad breath you smell is the exhaust fume from a biological engine of destruction that has established a foothold in your pet’s mouth.
But what if the key wasn’t masking the smell, but eliminating its source? The truth is that your pet’s mouth is a microbiome gateway to their entire body. By ignoring the health of this gateway, we are leaving the door wide open for systemic diseases that target the most vital organs. This isn’t about achieving a perfect smile; it’s about preventing silent inflammation and organ damage that starts with something as seemingly innocent as plaque.
This guide will walk you through the science of this mouth-body connection. We’ll explore how bacteria make the journey from gums to heart valves, debunk the myths surrounding popular dental “solutions,” and provide you with a clear, actionable plan to transform your pet’s oral health from a liability into an asset for a longer, healthier life.
In this article, we will dissect the critical aspects of your pet’s dental health, providing a clear path from understanding the problem to implementing effective, life-extending solutions.
Summary: Your Complete Guide to Pet Dental Health and Longevity
- How Bacteria from Gums Travel to Heart Valves in Small Breed Dogs?
- How to Train an Adult Dog to Accept Tooth Brushing in 4 Weeks?
- Anesthesia-Free Dentistry vs. Professional Cleaning: Which is Safe?
- The “Dental Chew” Myth: Why 80% of Treats Don’t Clean Below the Gumline
- When to Book a Dental Exam: 3 Subtle Signs Your Cat Is in Mouth Pain
- Large Breed Puppy Food: Why Is Lower Protein Density Crucial for Joints?
- What Actually Happens During a 30-Minute Wellness Exam That Justifies the Fee?
- How to Train an Adult Dog to Accept Tooth Brushing in 4 Weeks?
How Bacteria from Gums Travel to Heart Valves in Small Breed Dogs?
The journey from a little bit of plaque to a life-threatening heart condition is shorter and more direct than most owners imagine, especially in small breed dogs. It all begins with gingivitis—inflamed, bleeding gums caused by bacterial biofilm. This inflammation compromises the integrity of the gum tissue, turning it into a porous entry point to the bloodstream. Think of it as a security breach at the body’s most vulnerable border crossing: the oral microbiome gateway.
Once in the bloodstream, these oral bacteria embark on a process called bacteremia. They travel throughout the body, but they have a particular affinity for certain sites. For reasons we are still studying, they are especially drawn to the heart valves. The turbulent blood flow around the valves creates an environment where these bacteria can easily attach and colonize, a process known as bacterial seeding. They form vegetative growths on the valve leaflets, leading to a serious condition called endocarditis. This infection physically damages the heart valves, impairing their ability to open and close properly and ultimately leading to heart failure.
This isn’t a rare occurrence. According to VCA Canada, an alarming 80% of dogs over three years old suffer from active dental disease, with small and brachycephalic (flat-faced) breeds being at significantly higher risk due to tooth crowding. This visual below helps conceptualize the microscopic invasion that happens every day in an unhealthy mouth.
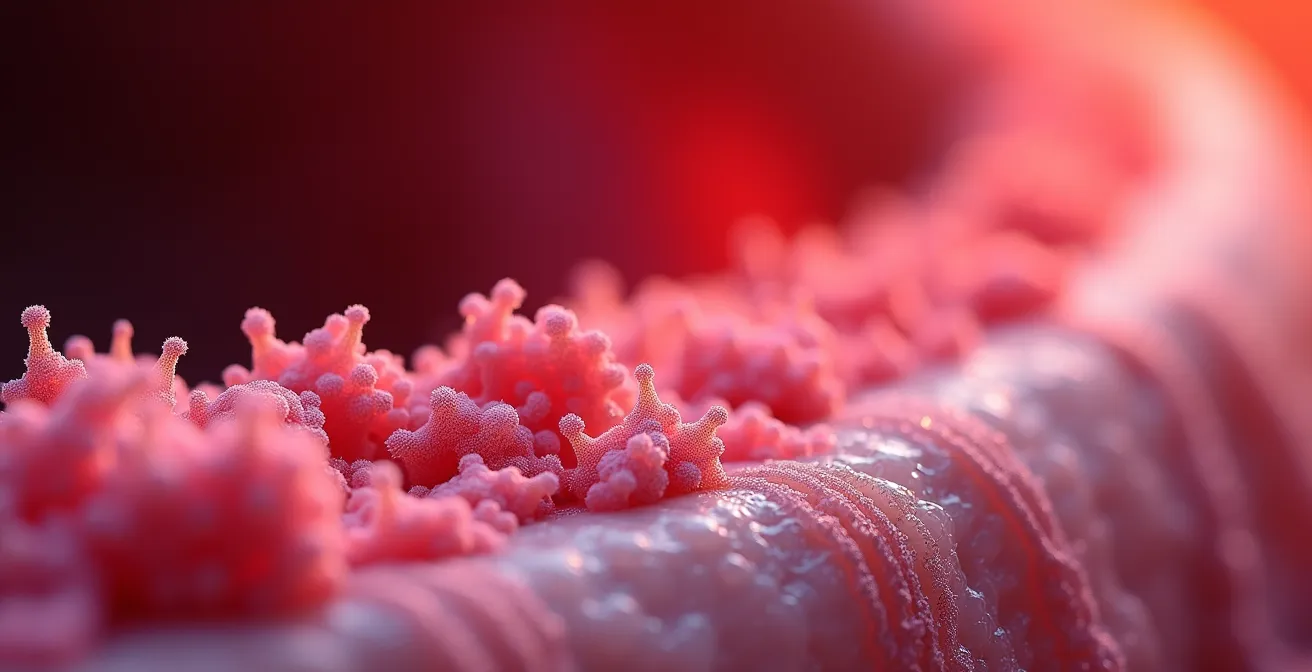
As this microscopic view illustrates, the bacterial biofilm is a complex, living community. When it’s allowed to thrive below the gumline, it triggers chronic, silent inflammation that not only damages the mouth but sends inflammatory signals throughout the body, affecting the kidneys and liver as well. As experts from VCA Canada Hospitals state, “Bacteria from dental infections can enter the bloodstream and potentially affect vital organs such as the heart, liver, and kidneys.” Ignoring dental health is not a passive act; it’s actively allowing this dangerous migration to happen.
How to Train an Adult Dog to Accept Tooth Brushing in 4 Weeks?
The single most effective tool against the bacterial invasion we’ve discussed is a simple, soft-bristled toothbrush. Daily brushing is the gold standard for disrupting the sticky biofilm before it can mineralize into hard tartar and open the microbiome gateway. But many owners of adult dogs give up, believing their pet is “too old” or “too stubborn” to learn. This is a myth. With patience and a positive approach, you can build a successful brushing routine.
The key is to reframe the goal from “cleaning their teeth” to building a cooperative care mindset. This isn’t a battle to be won; it’s a new activity to learn together. The process should be gradual, positive, and always end on a good note before your dog gets stressed. Using a highly palatable, enzymatic pet toothpaste (never human toothpaste) makes the experience a rewarding treat, not a punishment. The goal of the first week isn’t to brush, but simply to introduce the taste in a happy context.
This approach has been proven effective time and again. The Ontario SPCA’s dental health program, for instance, focuses on positive reinforcement to prepare shelter animals for their new homes. Their program successfully trained over 85% of adult rescue dogs to accept tooth brushing within 30 days using these gradual techniques. This dramatically reduced dental disease rates in adopted animals, proving that it’s never too late to start.
The following four-week plan, adapted from guidelines by veterinary experts at Cornell University, breaks the process down into manageable steps. Remember to keep sessions short (1-2 minutes) and full of praise.
- Week 1: The Introduction. Offer a small amount of pet-specific toothpaste on your finger. Let your dog lick it off. Repeat daily, praising them enthusiastically. The goal is to associate the flavour with a positive reward.
- Week 2: Finger Brushing. After they eagerly lick the paste from your finger, begin to gently rub your finger over the outside of their gums and front teeth. Don’t force their mouth open. Just lift their lip. Focus on the front canines and incisors.
- Week 3: Introducing the Brush. Put toothpaste on a soft pet toothbrush and let your dog lick it off the bristles. Don’t brush yet. Let them investigate the tool and learn it’s another source of the tasty paste.
- Week 4: The First Brush. Start making gentle, circular brushing motions on the outside of the front teeth for just a few seconds. Gradually increase the duration to 30 seconds over the week. Focus on the outer surfaces, as this is where most tartar accumulates.
Anesthesia-Free Dentistry vs. Professional Cleaning: Which is Safe?
As awareness of dental health grows, a tempting alternative has emerged: anesthesia-free dentistry. Offered by some groomers and laypersons, it promises a cheaper, “safer” way to clean a pet’s teeth by avoiding general anesthesia. As a veterinary professional, I must be unequivocal: this practice is not only ineffective, but it is dangerous and creates a false sense of security that can have devastating consequences.
The core danger lies in what these procedures *cannot* do. The most critical part of a dental cleaning happens below the gumline (subgingivally), where periodontal disease takes root. Anesthesia-free cleaning only scrapes the visible tartar off the tooth crown—a purely cosmetic procedure. This is like cleaning only the tip of an iceberg. The true threat remains hidden, allowing the disease to progress silently. Furthermore, it’s impossible to perform a thorough oral exam, take dental X-rays to check for bone loss or root abscesses, or polish the teeth to prevent rapid plaque re-attachment on a conscious, anxious animal.
A professional dental cleaning, or Comprehensive Oral Health Assessment and Treatment (COHAT), is a meticulous medical procedure. Your pet is safely placed under general anesthesia with dedicated monitoring of their vital signs, just like a human patient. This allows the veterinary team to clean, probe, and X-ray every single tooth surface without causing pain or stress. As renowned veterinary dentist Dr. Jan Bellows states, “Cleanings that don’t use anesthesia may sound appealing, but they only remove surface tartar and can cause pain or injury. Worse, they miss problems hiding under the gums.”
The American Veterinary Medical Association (AVMA) has taken a strong stance against this practice. The following table, based on their guidelines, highlights the critical differences. This isn’t a matter of opinion; it’s a matter of medical standards and patient safety.
The following table, based on data and recommendations from the American Veterinary Medical Association (AVMA), clearly outlines the critical differences and why one is a medical procedure and the other is a cosmetic compromise.
| Aspect | Anesthesia-Free | Professional (Under Anesthesia) |
|---|---|---|
| Below gumline cleaning | Not possible | Complete cleaning |
| Dental X-rays | Cannot be performed | Full mouth radiographs |
| Pain management | None available | Full pain control |
| Disease detection | Surface only | Complete oral exam |
| Safety for pet | Risk of injury/stress | Monitored & controlled |
| AVMA recommendation | Not recommended | Gold standard |
The “Dental Chew” Myth: Why 80% of Treats Don’t Clean Below the Gumline
The pet store aisles are filled with products promising to clean your dog’s teeth and freshen their breath. Dental chews, bones, and biscuits are a multi-million dollar industry built on the promise of an easy fix. The myth is that chewing any hard treat is enough to maintain oral health. The reality is that the vast majority of these products do very little to address the root cause of periodontal disease: the subgingival biofilm.
Effective cleaning relies on two principles: mechanical abrasion to scrape away plaque, and a chemical action to inhibit bacteria. Most standard biscuits or hard chews are too brittle. They shatter on impact or are swallowed too quickly to provide any meaningful friction against the tooth surface, especially near the gumline. Even worse, some products like real bones, antlers, or hard nylon toys are so hard that they frequently cause painful and expensive tooth fractures. They “clean” the tooth by breaking it.
This is where the Veterinary Oral Health Council (VOHC) becomes an essential guide for Canadian pet owners. The VOHC is an independent organization that evaluates pet products to see if they live up to their dental claims. To earn the VOHC Seal of Acceptance, a product must scientifically prove its effectiveness. It’s not a paid endorsement; it’s a certification based on evidence. According to their standards, only products that are proven to reduce plaque or tartar by at least 20% receive this seal. When you see the VOHC seal, you know the product has passed rigorous testing.

Looking at the different textures, it becomes clear that not all chews are created equal. Products with the VOHC seal often have a unique flexible texture, ridges, or nubs designed to wrap around the tooth and scrape down to the gumline as the dog chews. They work by prolonging chew time and maximizing surface contact to disrupt the biofilm. They are a helpful supplement to daily brushing, but never a replacement for it.
Your VOHC Shopping Checklist: How to Choose Safe Dental Products
- Seek the Seal: Before purchasing any dental chew or diet, look for the VOHC (Veterinary Oral Health Council) seal on the packaging. This is your primary assurance of effectiveness.
- Check for Size: Always choose the appropriate size chew for your dog’s body weight. A chew that is too small is a choking hazard.
- Supervise the Session: Never leave your dog unattended with a dental chew. Supervise all chewing sessions to ensure they are consuming it safely and not trying to swallow large pieces.
- Perform the Fingernail Test: Avoid any chew that is too hard. A good rule of thumb is the fingernail test: if you cannot press your nail into the surface of the chew, it’s likely hard enough to fracture a tooth. Avoid antlers, hooves, and hard nylon bones.
- Introduce Slowly: When introducing a new dental chew, start with reduced portions and monitor your pet for any signs of gastrointestinal upset.
When to Book a Dental Exam: 3 Subtle Signs Your Cat Is in Mouth Pain
While dogs are often the focus of dental discussions, cats suffer from periodontal disease at similar rates, but with a dangerous difference: they are masters at hiding their pain. As both predator and prey animals, showing weakness is a survival liability. A cat can be suffering from excruciating mouth pain from resorptive lesions or severe gingivitis and still continue to eat, purr, and appear “normal” to even the most loving owner.
This is why waiting for obvious signs like dropping food or crying out in pain is often too late. By the time a cat displays such clear distress, the underlying disease is typically advanced and may require multiple, complex extractions. As a veterinarian, my plea to cat owners is to stop looking for obvious pain and start looking for subtle changes in behaviour. These are the real cries for help.
A Canadian veterinary study provided valuable insights into this challenge. VCA Canada reports that while more than 50% of cats over age 3 have dental disease, most show no outward signs. However, in their clinical observations of cats later diagnosed with painful dental conditions, a pattern of subtle changes emerged. After receiving necessary dental treatment, an incredible 60% of these cats showed significant positive behavioral improvements, with owners often remarking their cat was acting “like a kitten again.”
Case Study: The Three Subtle Signs of Feline Oral Pain
Based on clinical data from the VCA Canada study and feline veterinary consensus, the three most common yet subtle signs of mouth pain in cats are not what you’d expect. Instead of overt signs, look for these behavioural shifts:
- Preference for One Side of the Food Bowl: A cat may consistently eat from only the left or right side of their bowl, or tilt their head in a specific way to chew. This is an attempt to avoid a painful area in their mouth.
- Decreased Grooming or Matted Fur: Grooming can be painful for a cat with a sore mouth. You might notice their coat becoming unkempt, greasy, or even matted, particularly over their back and hindquarters where it’s harder to reach.
- Hesitation Before Jumping: A jolt of pain can occur upon landing from a jump. You might notice your once-agile cat hesitating before jumping up onto a counter or down from a chair, or choosing to take a lower route instead.
Large Breed Puppy Food: Why Is Lower Protein Density Crucial for Joints?
While this article focuses on dental health, the foundation for a lifetime of wellness—including oral wellness—is laid in puppyhood. For large and giant breed puppies (like Great Danes, Golden Retrievers, or Bernese Mountain Dogs), nutrition has a profound and immediate impact on their skeletal development. Feeding them standard puppy food can be a critical mistake. Their growth must be carefully managed to prevent developmental orthopedic diseases like hip dysplasia.
The key is controlled growth. Large breed puppy formulas are specifically designed with lower energy density and carefully balanced mineral levels. They have slightly lower protein and fat, and most importantly, a strictly controlled calcium-to-phosphorus ratio. This prevents them from growing too quickly, which puts excessive strain on their developing joints and soft growth plates. Rapid growth can lead to permanent damage and a lifetime of arthritis pain.
But how does this connect to dental health? The answer lies in the food’s physical form and the habits it establishes. The kibble in large breed puppy food is not just a vessel for nutrients; it’s your puppy’s first toothbrush. The larger, often more porous kibble size is designed to encourage chewing rather than swallowing whole. This mechanical abrasion provides a daily, gentle cleaning action that helps reduce plaque accumulation from the moment their adult teeth erupt.
By choosing the right food from the start, you are establishing a dual benefit: protecting their joints and initiating a passive dental care routine that will serve them for life. As many experienced Canadian owners can attest, this foundational choice pays dividends.
Large breed puppy owners report that appropriate kibble size not only supports controlled growth but provides essential mechanical cleaning action. Choosing Canadian-made foods with proper calcium/phosphorus ratios and dental-friendly kibble design helps establish lifelong oral health habits from puppyhood.
– Canadian Large Breed Owner Experience, Pet Food Institute
What Actually Happens During a 30-Minute Wellness Exam That Justifies the Fee?
The annual or semi-annual wellness exam can sometimes feel like a quick, expensive visit. Your veterinarian weighs your pet, feels their belly, listens to their heart, gives a few vaccines, and sends you on your way. Many owners wonder what they’re truly paying for. The answer is expertise and early detection. That 30-minute exam is a systematic search for the subtle signs of disease, and nowhere is this more critical than in the oral cavity.
A huge portion of that exam’s value is the conscious oral assessment. While your pet is awake, your veterinarian is performing a multi-point inspection that you cannot do at home. They are lifting the lips to assess tartar levels, checking for fractured teeth, looking for the tell-tale red line of gingivitis along the gums, and palpating the jaw and lymph nodes for signs of swelling or asymmetry that could indicate an abscess or oral tumour. This is the moment where the earliest stages of periodontal disease are caught.
This early detection is not just a health benefit; it’s a significant financial one. In fact, the Canadian Veterinary Medical Association highlights the stark economic reality of proactive versus reactive care. By age three, 80% of dogs and cats show signs of periodontal disease. Detecting this at a Grade 1 or 2 stage during a wellness exam allows for a routine preventative cleaning. Waiting until the disease is advanced (Grade 3 or 4) can lead to the need for complex surgical extractions and advanced periodontal treatments that can easily exceed $2,000.
By age three, 80% of dogs and cats show signs of periodontal disease. Early detection during wellness exams can help you avoid over $2,000 in advanced periodontal surgery.
– Canadian Veterinarian Medical Association, Petsecure Dental Month Campaign
To maximize the value of this exam, you must be an active participant. Your observations at home are a vital part of the diagnostic process. Arrive prepared to discuss any changes you’ve noticed and don’t be afraid to ask specific questions about your pet’s dental health. Use your veterinarian’s expertise to its fullest.
- Can you grade my pet’s dental health on the 0-4 periodontal disease scale today?
- Based on their breed and age, what preventative dental strategy do you recommend?
- Can you show me any tartar buildup or gum inflammation you’re seeing?
- When should we schedule their next professional dental cleaning?
- Does my pet insurance in Canada cover preventative dental care or only treatment for accidents and illness?
Key Takeaways
- Bad breath is not normal; it’s the primary sign of an oral infection that can spread to the heart, kidneys, and liver.
- Daily tooth brushing is the gold standard for prevention. Anesthesia-free cleaning is a cosmetic procedure that fails to address disease below the gumline.
- Look for the VOHC seal on dental chews to ensure they are scientifically proven to be effective, and avoid items hard enough to fracture teeth.
How to Train an Adult Dog to Accept Tooth Brushing in 4 Weeks?
We’ve established the four-week plan to introduce tooth brushing, but the most common point of failure isn’t the dog—it’s the owner’s mindset. If you approach brushing as a chore you have to “get done” or a fight you have to “win,” your dog will sense your stress and resistance, and the process is doomed. The secret to success lies in shifting to a cooperative care mindset. This is not about forcing compliance; it’s about patiently teaching a new skill and building trust.
Your goal for the first few weeks is simply to create a positive association. The toothpaste should be a high-value treat. The session should be short, happy, and always end before your dog shows signs of stress (like turning their head away, yawning, or licking their lips). If you push them past their comfort zone, you create a negative memory that makes the next session harder. If they resist, simply end the session with a “Good dog!” and try again tomorrow for a shorter duration. Consistency over intensity is the rule.
Think of it like teaching a child to tie their shoes. You wouldn’t expect them to get it on the first try. You’d break it down into small steps, celebrate the small wins, and offer encouragement, not frustration. The same applies here. You are your dog’s trusted teacher. Your calm, positive energy is the most important tool you have. Every short, successful interaction builds a foundation of trust that makes future healthcare procedures, from nail trims to vet exams, easier for everyone.
This is not just a theory; it is a proven methodology used by animal professionals everywhere to rehabilitate and train even the most fearful animals. The success of the Ontario SPCA program with adult rescue dogs is a powerful testament to this fact. They proved that with the right approach, even animals with unknown histories can learn to participate happily in their own care. Your dog, who already trusts you, has an even greater capacity to learn.
By embracing this preventative mindset, you are not just cleaning their teeth; you are actively closing the gateway to systemic disease. The next logical step is to book their annual wellness exam and have a frank discussion with your veterinarian about scheduling their first professional comprehensive oral health assessment.
Frequently Asked Questions About Pet Dental Health
Why don’t cats show obvious pain signs like dogs?
Cats are masters at hiding pain as a survival instinct. They may still eat normally despite severe dental disease, making regular exams crucial.
What is tooth resorption in cats?
Nearly 70% of cats experience resorptive lesions – painful holes in tooth enamel that require extraction. It’s often only detected through dental X-rays.
How often should indoor Canadian cats have dental exams?
Annual dental assessments are minimum; cats over 7 years may benefit from twice-yearly checks due to increased risk of dental disease.